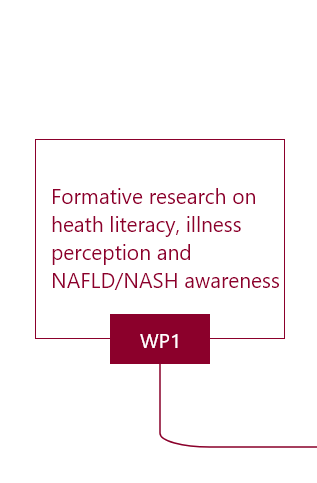
WP1 Formative research on heath literacy, illness perception and NAFLD/NASH awareness.
Background
Patient health literacy, illness perception and awareness are key factors driving health behaviour with important implications for doctor-patient interaction, risk communication and, subsequently, care provision.
Objectives
- To assess Health Literacy, illness perception and NAFLD/NASH awareness in high-risk primary care patients in Greece, Spain and the Netherlands.
- To explore how communication pathways affect risk perception for improving provider communication skills.
Methods
In a descriptive study, a total of 840 patients with age ≥50 years and obesity or Metabolic Syndrome or Type 2 Diabetes Melitus, consecutively visiting primary care practices, will be selected to complete CRF assessing socio-demographic characteristics, health habits and biomedical indexes. Health Literacy, illness perception and NAFLD/NASH awareness will be assessed using the European Health Literacy Survey Questionnaire, the Brief Illness Perception Questionnaire and the Public Awareness of NAFLD Questionnaire respectively. Findings will be complemented by literature review on risk communication pathways. Descriptive statistics and univariate/multivariate tests will be used for analysis.
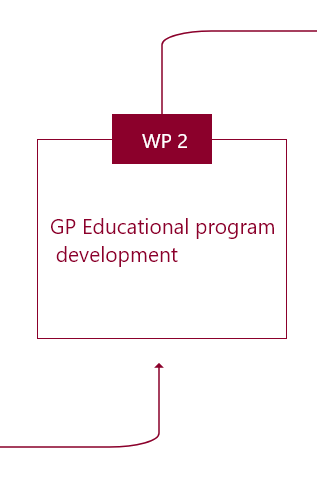
WP2 Development of an educational module for NAFLD/NASH in primary care.
Background
Despite the increasing prevalence of NAFLD, there is limited knowledge and practice regarding its staging, diagnosis and management in primary care.
Objectives
- To develop an evidence-based educational module for NAFLD/NASH addressed to primary care professionals in Greece, Spain and the Netherlands.
- To adapt the educational module to local cultural and clinical practice contexts.
Methods
Using information generated from WP1 and the latest clinical knowledge, an expert panel of primary care professionals and specialists will develop module key messages, learning objectives and content, including the following topics:
The training content will be locally adapted and translated to Greek, Spanish and Danish to maximize value to recipients. The module will be designed for delivery primarily via e-learning and we will seek accredited by the European Accreditation Council for Continuing Medical Education (EACCME).
- What is NAFLD/NASH and what is its natural history?
- Why is NAFLD/NASH an important issue for primary care?
- Who is at risk and who will be screened?
- NAFLD/NASH staging?
- NAFLD/NASH diagnosis?
- NAFLD/NASH management
The training content will be locally adapted and translated to Greek, Spanish and Danish to maximize value to recipients. The module will be designed for delivery primarily via e-learning and we will seek accredited by the European Accreditation Council for Continuing Medical Education (EACCME).
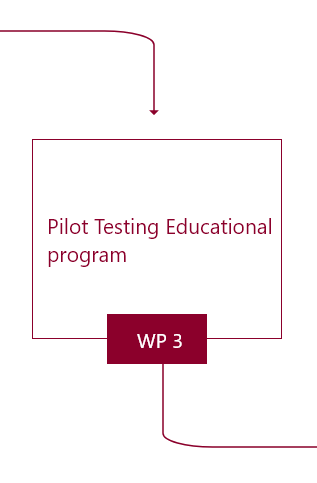
WP3 Evaluation of a NAFLD/NASH educational intervention in primary care practice settings
Background
Evaluation is important for examining the impact of training on clinician’s knowledge, attitudes, skills, confidence and practice and can be used for training refinement.
Objectives
To pilot test in a sample of primary care professionals the:
- Impact of an NAFLD/NASH educational intervention on primary care providers in Greece, Spain and the Netherlands.
- Acceptability and provider satisfaction with the educational intervention;
Methods
A before-and-after, cross-sectional pilot study will be conducted. A random sample of primary care professionals (n=50) per country (total n=150), stratified by years of experience, geographic setting and work on private/public domain, will be selected.
Outcome measures will be:
We will also evaluate trainee satisfaction and perceived training added value.
Measurement will occur pre, post and one month following the training.
Qualitative research will be used to assess intervention practicability and acceptability (five primary care professionals per country will be selected for a semi-structured telephone interview). Descriptive statistics and univariate/multivariate models will be used.
Country-level differences will be examined.
Outcome measures will be:
- change in key knowledge related to NAFLD,
- screening,
- risk perception,
- self-efficacy and self-reported changes to five clinical practice areas.
Measurement will occur pre, post and one month following the training.
Qualitative research will be used to assess intervention practicability and acceptability (five primary care professionals per country will be selected for a semi-structured telephone interview). Descriptive statistics and univariate/multivariate models will be used.
Country-level differences will be examined.
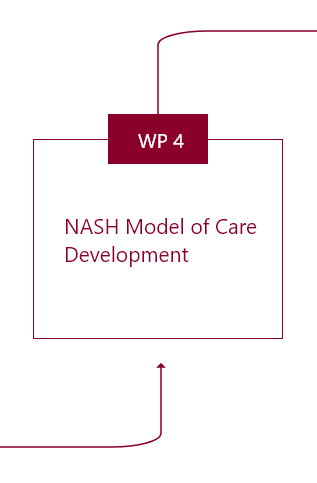
WP4 Development and pilot testing of an evidence-based model of care for NAFLD/NASH management in primary care.
Background
Guidance on NAFLD/NASH screening based on availability of diagnostic tests within primary care systems is currently lacking. Best-practice criteria can help with addressing bottle necks. In this WP, a model of care will be developed for use in primary care to enhance NAFLD/NASH screening, diagnosis and linkage to specialty care.
Objectives
- To develop an evidence-based NAFLD/NASH model of care to guide NAFLD/NASH management in primary care.
- To adapt the model of care to cultural and clinical practice contexts of Greece, Spain and the Netherlands.
Methods
Model development will follow the Plan-Do-Study-Act framework and knowledge of previous WPs. The model will include a standardized care pathway where different tasks will be defined, optimized and sequenced. This will systematically identify and follow patients at risk for NAFLD/NASH, beginning from primary care, aiming to improve care quality and efficiency, health professionals coordination/cooperation and patient satisfaction.
TThe following model elements be addressed:
Two primary care professionals in each country will be trained to pilot test the draft model of care (n=20 patients per country) to address content, feasibility and adherence.
TThe following model elements be addressed:
- evidence-base;
- risk assessment;
- model objectives and prioritization criteria;
- patient journey mapping;
- pathway algorithm implementation tools and supportive materials;
- patient education and self-management.
Two primary care professionals in each country will be trained to pilot test the draft model of care (n=20 patients per country) to address content, feasibility and adherence.
WP5 Evaluating a clinical model of care for the screening, diagnosis and treatment of NAFLD/NASH among primary care patients.
Background
Model evaluation is necessary for establishing model effectiveness, including factors related to process, outcomes and feasibility. Model evaluation will guide necessary adjustments for achieving optimal adaptation, impact and integration.
Objectives
- To evaluate the impact of a NAFLD/NASH model of care on NAFLD/NASH screening, diagnosis and linkage to specialty care.
- To evaluate the model’s process effectiveness.
- To assess the model’s acceptability and practicability.
Methods
A pre-post randomized controlled study design will be conducted.
Twelve primary care practices (4 practices per country) will be selected to participate in model evaluation. Practices will be randomized to ‘intervention’ and ‘control’ groups in a 1:1 ratio. From each practice 50 patients at high risk for NAFLD/NASH (age >50 years, obesity, T2 Diabetes Mellitus or Metabolic Syndrome) will be recruited. Screening algorithms will include serum biomarkers and calculation of FIB-4.
In the active group, participants will be exposed to the Model of Care developed in WP4. In the control group, participants will receive usual care. Outcomes will be assessed in both arms.
Primary outcomes include the numbers of patients screened, diagnosed with advanced fibrosis and referred to specialists.
Secondary outcomes include proportions of patients accepting assessment at primary care (process evaluation), accepting referral to specialists (process evaluation), without advanced fibrosis (F1/F2) not needing referral, with advanced fibrosis (F3/F4) receiving comprehensive care, numbers of high-risk patients screened for NAFLD/NASH allocated to primary care and costs of model implementation.
Additional patient data include: socio-demographics, health habits, biomedical indexes, personal and family history, laboratory tests and hepatic testing.
Electronic medical records will be used to track patient outcomes. Semi-structured interviews and focus groups will also be conducted with purposively selected patients (n=10 per country) and stakeholders to explore communication pathways, integrated care provision, patient and provider satisfaction. Patient-level characteristics and model delivery rates will be compared between pre/post assessments and between active and control groups.
Qualitative outcomes will be analyzed using Thematic Content Analysis.
Twelve primary care practices (4 practices per country) will be selected to participate in model evaluation. Practices will be randomized to ‘intervention’ and ‘control’ groups in a 1:1 ratio. From each practice 50 patients at high risk for NAFLD/NASH (age >50 years, obesity, T2 Diabetes Mellitus or Metabolic Syndrome) will be recruited. Screening algorithms will include serum biomarkers and calculation of FIB-4.
In the active group, participants will be exposed to the Model of Care developed in WP4. In the control group, participants will receive usual care. Outcomes will be assessed in both arms.
Primary outcomes include the numbers of patients screened, diagnosed with advanced fibrosis and referred to specialists.
Secondary outcomes include proportions of patients accepting assessment at primary care (process evaluation), accepting referral to specialists (process evaluation), without advanced fibrosis (F1/F2) not needing referral, with advanced fibrosis (F3/F4) receiving comprehensive care, numbers of high-risk patients screened for NAFLD/NASH allocated to primary care and costs of model implementation.
Additional patient data include: socio-demographics, health habits, biomedical indexes, personal and family history, laboratory tests and hepatic testing.
Electronic medical records will be used to track patient outcomes. Semi-structured interviews and focus groups will also be conducted with purposively selected patients (n=10 per country) and stakeholders to explore communication pathways, integrated care provision, patient and provider satisfaction. Patient-level characteristics and model delivery rates will be compared between pre/post assessments and between active and control groups.
Qualitative outcomes will be analyzed using Thematic Content Analysis.
WP6 Development of harmonized set of NAFLD/NASH guidelines for primary care.
Background
The joint EASL-EASD-EASO Clinical Practice Guidelines on NAFLD management proposed recommendations for patient diagnosis, treatment and follow-up. This work package will involve the update of the existing guidelines tailored with specific recommendations for NAFLD/NASH management in primary care.
Objectives
- To harmonize NAFLD/NASH guidelines for primary care
Methods
This will be a consensus-based approach. The process will involve multidisciplinary teams, expert meetings, literature review, quality assessment and drafting, grading and consolidating recommendations (consensus reports). Existing guidelines, the results of previous project WPs and expert opinion will be the three main sources of information for guideline adaptation. Expert panels with representatives from EASD, EASO and ESPCG will be conducted. The guidelines will offer a hierarchy of recommendations and evidence for screening and diagnosis to allow for selection based on local resources. A refined NAFLD/NASH pathway will also be presented with the guideline recommendations to assist with the operationalization into real world practice settings.